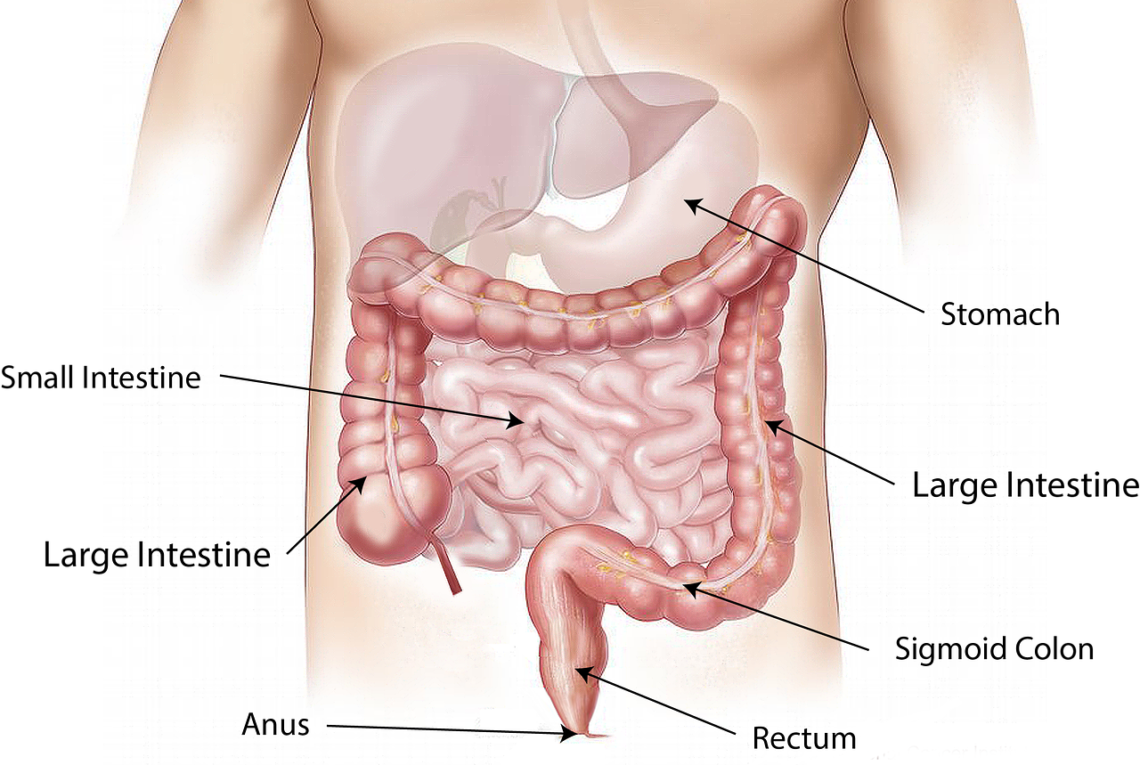
The anal canal is the final part of your large intestine. It runs downwards and backwards from the anorectal junction to the anus. It is surrounded by inner involuntary and external voluntary sphincters to control the evacuation of feces.
It is distinguished from the rectum by a transition along its internal surface from endodermal to skin-like ectodermal tissue.
The length of the anal canal
The anal canal is the last part of your colon that is surrounded by important muscles (anal sphincters) that control bowel movements. Food travels through your large intestine and by the time it gets to your anus, it has been reduced to solid waste that is ready to leave the body. The anal canal acts as a holding area for this waste until it is released by the anal sphincters during defecation.
The proximal portion of the anal canal is lined by the columnar epithelium that lines your rectal mucosa. This epithelium transitions at the point of the dentate line, also known as the pectinate line, to non-keratinized stratified squamous epithelium. This is called the anal transition zone (ATZ).
The muscular anal canal forms a tube that extends from the anorectal junction to your anus and contains muscles that are similar to those that control your urinary bladder and urethra. The anal canal is also surrounded by the internal and external anal sphincters that, when relaxed, allow stool to leave the body during defecation.
The anatomy of the anal canal
The anal canal is the terminal part of the digestive tract. It is 2.5 to 4 cm (1 to 1.5 inches) long and lies entirely extraperitoneally, beginning distal to the rectal ampulla at the anorectal line. It is surrounded by the inner involuntary and outer voluntary sphincters that control evacuation of feces.
Like the rectum, it is lined with mucosa. In the upper portion, this is organised into longitudinal folds called anal columns and separated from each other by furrows called anal sinuses. Each of these sinuses open to glands that secrete lubricating mucus. At the inferior end of the anal canal are small circular valve-like folds called anal valves, which join together the lower ends of the anal columns.
In the transition zone between these two areas, a layer of epithelium known as the anal verge forms. This blends with connective tissue from the muscular coat of the recum and is a precursor to the skin of the anus and perianal area.
Behind the anal canal are, in males, the seminal vesicles, prostate and urethra; in females, the cervix and vagina with the perineal body in between. In front of the anal canal is a mass of muscular and fibrous tissue, the coccyx or pelvic diaphragm. Behind this is a rich presacral plexus of veins. The anal canal is connected to the coccyx by the anococcygeal ligament.
The function of the anal canal
The anal canal is a vital part of the body that conveys stool from the rectum to the anus. It also helps to maintain faecal continence. It is often subject to enlargement and irritation, known as haemorrhoids. Haemorrhoids can occur in the anal canal as a result of constipation, straining during defecation and raised intra-abdominal pressure. They are made up of vascular cushions that contain mucus-producing cells, and are sensitive to pain, touch and temperature.
The upper two thirds of the anal canal is lined with columnar epithelium – similar to the lining of the rectum. However, further down the anal canal the epithelium changes to squamous cells. This change is marked by a line called the pectinate or dentate line. This line demarcates the superior two-thirds of the anal canal derived from the endodermal hindgut, and the inferior one-third derived from the ectodermal proctodeum.
When you feel the urge for a bowel movement your brain signals to the internal anal sphincter muscles to relax, allowing stool to pass into the anal canal. From there, it is pushed out the anus during defecation. The anal canal has an important role in the immune system as it defends against organisms entering the rectal area and helps to differentiate between solid, liquid and gaseous faeces. The anal canal also protects the genitals from infection and is a site for sexually transmitted diseases such as HPV.
The treatment of anal stenosis
The anal canal is a slit-like passage through the rectum that extends from the anorectal junction to the anus. It is surrounded by inner involuntary and outer voluntary sphincters, and it contains vertical mucosal folds called anal columns or sinuses of Morgagni. It is sensitive to pain, pressure and temperature. The anal canal is also the location of pathological haemorrhoids, which can be painful and itchy.
The diagnosis of anal stenosis is usually made by physical examination and digital rectal exam. The doctor may also order an anorectal manometry, which is a test that measures the pressures of the internal and external sphincters during bowel movements.
There are a number of surgical techniques that can be used to treat anal stenosis. These techniques are based on the use of different flaps to reconstruct anal canal width and flexibility. Depending on the level of anal stenosis, these flaps can be classified as advancement, island, or rotational flaps [2] (Table 2).
Before surgery, patients should avoid drinking anything acidic and drink eight 8 oz glasses of water per day to reduce chances of developing postoperative bleeding. They should also not sit in a chair for more than ten days after surgery and try to wear loose clothing around the groin area. During the recovery period, patients should refrain from vigorous exercises and do not lift heavy objects.